Introduction
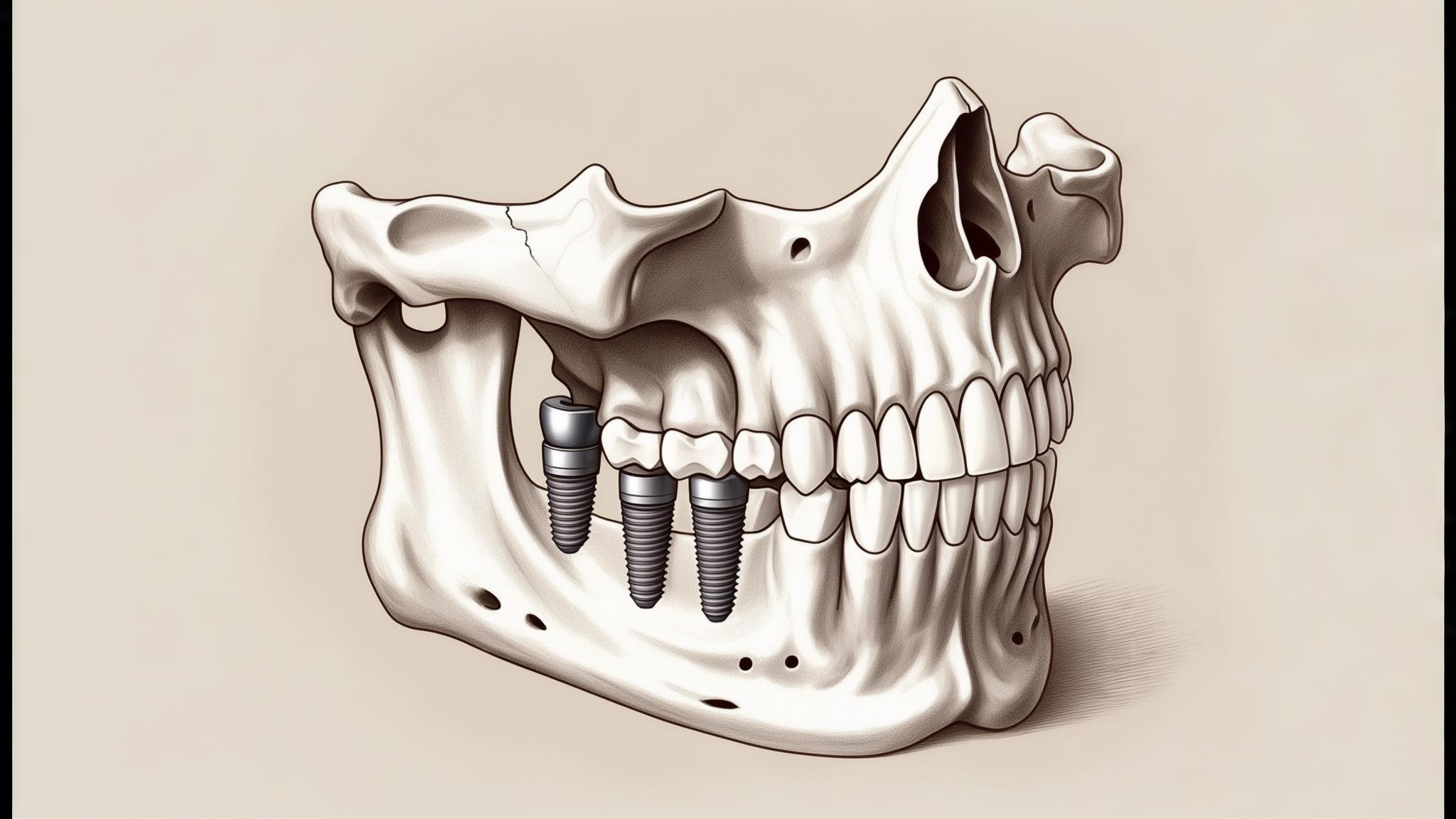
Dental implants are a revolutionary solution in restorative dentistry, offering a permanent replacement for missing teeth. They consist of a metal post surgically inserted into the jawbone, topped with a crown that mimics the look and function of a natural tooth. Implants are crucial for maintaining oral health, improving aesthetics, and enhancing the ability to chew and speak properly.
This article aims to delve into the nuances of dental implant procedures, especially focusing on the differences between the upper jaw (maxilla) and the lower jaw (mandible). Understanding these differences is key for both patients and dental professionals to ensure successful outcomes.
Overview of Dental Implants
Components of Dental Implants
Dental implants are composed of three main parts:
- Implant Post: This is a titanium screw that acts as the root of the tooth, anchoring the implant securely into the jawbone.
- Abutment: This component connects the implant post to the crown, serving as a base for the crown.
- Crown: The visible part of the implant, crafted to blend seamlessly with your natural teeth.
General Procedure for Dental Implants
The process of getting dental implants involves several stages:
- Initial Consultation and Imaging: The dentist conducts a thorough examination, often using X-rays or CT scans, to assess the jawbone's condition and plan the implant placement.
- Surgical Placement: The implant post is surgically inserted into the jawbone.
- Osseointegration Period: Over several months, the implant fuses with the bone in a process called osseointegration, providing a stable foundation.
- Abutment and Crown Placement: Once healed, the abutment is attached, and the custom-made crown is placed, completing the procedure.
Anatomy of the Upper Jaw (Maxilla) vs. Lower Jaw (Mandible)
Structural Differences
The maxilla and mandible differ significantly in terms of bone density and structure:
- Bone Density and Quality: The upper jaw generally has less dense bone compared to the lower jaw, which can affect implant stability.
- Shape and Size: The maxilla is typically thinner and more porous, while the mandible is denser and thicker.
Implications for Dental Implants
- Bone Volume Considerations: Adequate bone volume is crucial for implant stability, often requiring additional procedures in the upper jaw.
- Proximity to Sinuses: Implants in the upper jaw must consider the proximity to the sinus cavities, which can complicate placement.
Upper Jaw Implant Procedures
Specific Challenges in the Upper Jaw
- Sinus Proximity and Potential Complications: The upper jaw's closeness to the sinus cavities can pose risks of sinus perforation during implant placement.
- Bone Density Issues: The softer bone in the upper jaw may not support implants as readily, necessitating additional interventions.
Techniques Used in Upper Jaw Implant Procedures
- Sinus Lift Procedure: This technique elevates the sinus floor to create more bone space for the implant.
- Bone Grafting Options: Bone grafts are sometimes necessary to augment the bone volume, providing a solid foundation for the implants.
Success Rates and Outcomes for Upper Jaw Implants
While upper jaw implants can present challenges, modern techniques have significantly improved success rates. With proper planning and execution, outcomes are generally positive, ensuring patients regain full oral function and aesthetics.
Lower Jaw Implant Procedures
Characteristics of the Lower Jaw Conducive to Implants
- Generally Denser Bone: The denser bone structure of the mandible often supports implants more effectively.
- Easier Access for Surgery: The lower jaw is typically more accessible, simplifying surgical procedures.
Typical Procedures and Techniques Used
- Immediate Loading Options: In some cases, implants can be loaded with a temporary crown immediately after placement due to the mandible's stability.
- Fewer Additional Procedures Required: The lower jaw often requires fewer preparatory procedures, such as bone grafts, compared to the upper jaw.
Comparative Analysis of Upper and Lower Jaw Implant Procedures
Surgical Considerations
- Complexity of Procedures: Upper jaw procedures may be more complex due to sinus considerations and bone quality.
- Time Required for Healing and Osseointegration: The upper jaw may take longer to heal and integrate due to its structural characteristics.
Patient Experience and Recovery
- Pain Levels and Discomfort: Recovery experiences can vary, but proper pain management can mitigate discomfort.
- Duration of Recovery Time: The upper jaw may require a longer recovery period due to additional surgical steps.
Long-term Outcomes and Maintenance
- Success Rates Comparison: Both upper and lower jaw implants have high success rates with modern techniques, though the lower jaw typically fares slightly better due to its denser bone.
- Potential Complications Specific to Each Jaw: Understanding and planning for potential complications, such as sinus issues in the upper jaw, is crucial for long-term success.
Conclusion
In summary, while dental implants in the upper and lower jaws share common goals, they differ in complexity and approach due to anatomical differences. Individualized treatment planning is essential to address these unique challenges, ensuring optimal results for each patient.
Patients are encouraged to consult with dental professionals to tailor their treatment plans to their specific needs and conditions, ensuring a smooth and successful implant journey.
References
- Misch, C. E. (2014). Dental Implant Prosthetics. Elsevier Health Sciences.
- Buser, D., Chen, S. T., & Belser, U. C. (2008). Implant Placement in Postextraction Sites: A Literature Update. The International Journal of Oral & Maxillofacial Implants, 23(Suppl).
- Esposito, M., Grusovin, M. G., & Worthington, H. V. (2012). Interventions for Replacing Missing Teeth: Different Types of Dental Implants. Cochrane Database of Systematic Reviews.